Meningiomas are one of the most common forms of central nervous system tumors, but treatment modalities are currently limited to surgery and, in some cases, radiotherapy. New research has uncovered links between stem cell activity and meningioma growth, offering new ways to treat these tumors.
The Critical Importance of Meningioma Research
Thousands of women worldwide have been diagnosed with intracranial meningiomas after using birth control, particularly medroxyprogesterone acetate (Depo-Provera). By disrupting signalling between the hypothalamus, pituitary gland, and ovaries, Depo-Provera and similar birth controls may increase the risk of these tumors. It’s noted that approximately 70% of meningiomas express progesterone receptors, and the synthetic progesterone may exacerbate hormonally active meningioma tissue.
Pfizer has argued that it was not aware of these issues and cannot be held liable, but reports have suggested that Pfizer researchers knew of the risk since at least the 1980s and refused to disclose it for fear of losing revenue. This has left many women to suffer from severe headaches, vision problems, behavioral changes, or muscle weakness. Not only does this severely dismiss their quality of life, but it also results in costly and painful surgeries or experimental treatments.
While a Depo-Provera injury claim attorney can help victims receive compensation for their injuries, only clinicians and researchers can identify new ways to treat this disease without the need for invasive surgery or radiotherapy. Novel explorations into the role of stem cells in meningioma development are offering both greater insights and potential treatment avenues.
Understanding Meningioma Diversity Offers New Insights
In 2020, researchers at the University of California, San Francisco, completed a landmark study of meningiomas that found significant heterogeneity within individual tumors. High-grade, aggressive tumors demonstrated greater heterogeneity than low-grade tumors, which could explain why they may recur after recession and why certain treatment modalities fail.
One of the key findings of the study was that editing certain genes, including CDH2 and PTPRZ1, using CRISPR would slow or halt tumor growth, suggesting that gene editing, in conjunction with stem cell therapy, may prevent tumor recurrence.
Stem Cell Activity May Correlate to Tumor Recurrence
As noted by a study published in Neuro Oncology, meningiomas are typically benign, but around 20% are clinically regressive. These tumors recur even after recession, requiring additional surgeries and treatments.
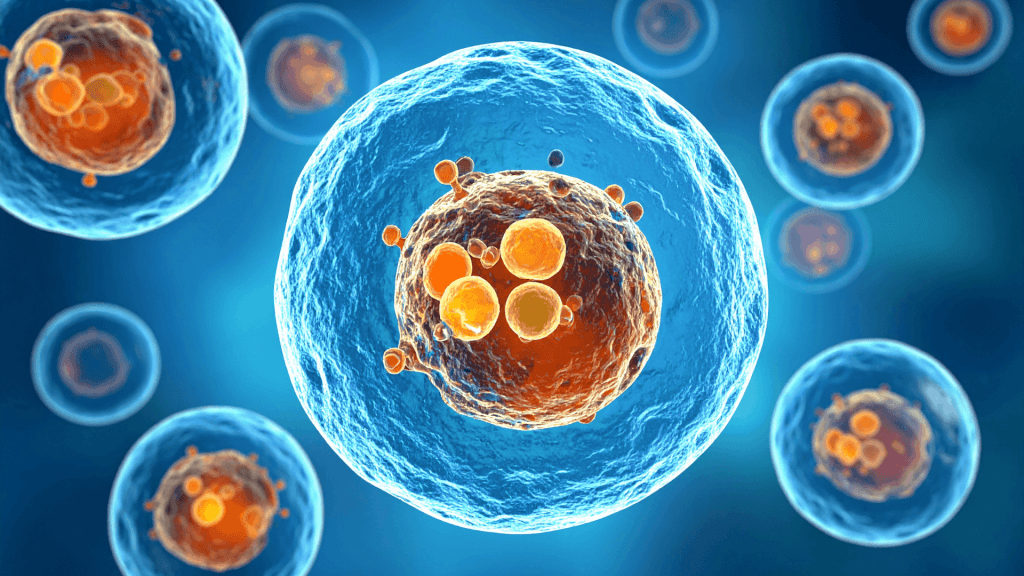
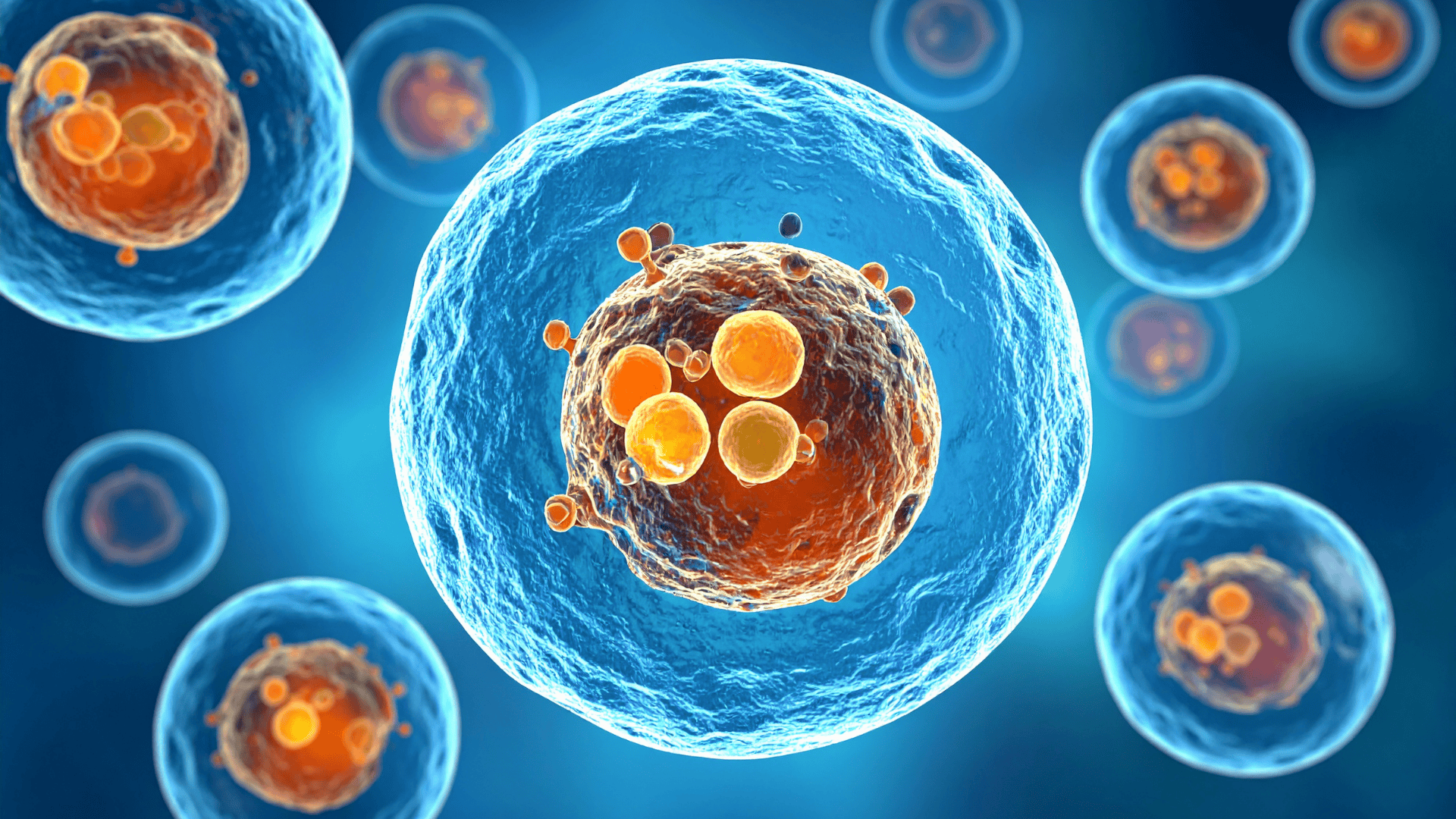
Researchers hypothesized that cancer stem cells may be present in these clinically benign tumors, with high responsiveness to the CXCL12-CXCR4/CXCR7 chemokine axis. Stem-like cells isolated from meningioma samples were under the control of the CXCR4/CXCR7 chemokine axis, which can explain their proliferation and resistance to treatment. The researchers suggested that CXCR4/CXCR7 antagonists may prove useful in inhibiting cell growth and preventing recurrence.
Research published in Clinical and Translational Oncology further explored the role of cancer stem cells in malignant meningiomas, a small but deadly subset of this tumor species. This study found that certain cancer stem cell biomarkers, namely Oct-4, Sox2, NANOG, and CD133, were associated with cell proliferation and drug resistance in meningiomas. CRISPR/Cas9 models also explored the pathways by which meningiomas proliferate. The researchers suggested that combination therapy, such as hydroxyurea alongside diltiazem, could improve patient outcomes.
Therapies for Brain Tumors: A Promising Avenue
Brain tumors are notoriously difficult to treat for several reasons. The blood-brain barrier prevents many chemicals from entering the brain, which may instead lead to toxic effects elsewhere in the body. High doses of radiation or chemotherapy can result in damage to healthy tissue and cause significant disruptions to the patient’s daily life.
Meningiomas and other tumors, such as glioblastomas, are notorious for recurring after resection due to “reseeding,” in which tiny tumor fragments are left behind to form new masses.
A 2016 article in Neuro Oncology noted that stem cells, when injected into brain tissue, will migrate toward the tumor site and can “home in” on migrating tumor cells, serving as trackers that can identify metastasis. This may provide novel tracking methods and allow for faster intervention.
Stem cell treatment, while still in its infancy for brain tumors, may be helpful. One promising avenue is direct cell reprogramming. This form of stem cell therapy takes the patient’s own stem cells and reprograms them into a new cell type, which can then proliferate as normal tissue would.
However, the development of these treatments has been fraught with issues, particularly around uncontrolled cell proliferation. Further research is needed to ensure safety and efficacy. New advancements in stem cell treatments, such as intranasal stem cell sprays, have offered hope for removing meningiomas.
A multifactorial approach to meningioma treatment, including stem cells and targeted drug therapy, can spare millions of patients from undergoing risky surgeries or suffering serious side effects from radiation treatment.
The heterogeneity, complexity, and location of meningiomas pose unique risks, and this tumor type has received less attention than others like glioblastomas. However, with meningioma diagnoses rising due to pharmaceuticals like medroxyprogesterone acetate, stem cell researchers have the potential to develop advanced treatments that reduce mortality and improve quality of life.

Pallavi Singal is the Vice President of Content at ztudium, where she leads innovative content strategies and oversees the development of high-impact editorial initiatives. With a strong background in digital media and a passion for storytelling, Pallavi plays a pivotal role in scaling the content operations for ztudium’s platforms, including Businessabc, Citiesabc, and IntelligentHQ, Wisdomia.ai, MStores, and many others. Her expertise spans content creation, SEO, and digital marketing, driving engagement and growth across multiple channels. Pallavi’s work is characterised by a keen insight into emerging trends in business, technologies like AI, blockchain, metaverse and others, and society, making her a trusted voice in the industry.